ASA 1
Normal healthy patient
ASA 2
Patient with mild controlled systemic disease which does not affect normal activity
ASA 3
Patient with severe systemic disease which limits activity
ASA 4
Patient with severe systemic disease which is incapacitating and is a constant threat to life
ASA 5
Moribund patient not expected to survive 24 hours with or without operation
Sunday, January 19, 2014
The American Society of Anesthesiologists (ASA) physical status classification system
Thursday, January 16, 2014
Sertoli Leydig cell tumour
The tumour is subdivided into many different subtypes. The most typical is composed of tubules lined by Sertoli cells and interstitial clusters of Leydig cells.
The prognosis is generally good as the tumour tends to grow slowly and usually is benign: 25% are malignant.
For malignant tumours with undifferentiated histology, prognosis is poor.
Sertoli-Leydig cell tumour is a group of tumours composed of variable proportions of Sertoli cells, Leydig cells, and in the case of intermediate and poorly differentiated neoplasms, primitive gonadal stroma and sometimes heterologous elements.
Sertoli-Leydig cell tumour is a member of the sex cord-stromal tumour group of ovarian and testicular cancers.
While the tumour can occur at any age, it occurs most often in young adults.
Recent studies have shown that many cases of Sertoli Leydig cell tumor of the ovary are caused by germline mutations in the DICER1 gene. These hereditary cases tend to be younger, often have a multinodular thyroid goiter and there may be a personal or family history of other rare tumors such as pleuropulmonary blastoma, Wilms tumor and cervical rhabdomyosarcoma.
Closely related terms include arrhenoblastoma and androblastoma. Both terms are classified under Sertoli-Leydig cell tumour in MeSH.
Presence of an ovarian tumour plus hormonal disturbances suggests a Sertoli-Leydig cell tumour. However, hormonal disturbance is present in only 2/3 of cases. A conclusive diagnosis is made via histology, as part of a pathology report made during or after surgery.
Wednesday, January 8, 2014
Potential Noncontraceptive benefits of hormonal contraception
Potential non-contraceptive benefits of hormonal contraception (American College of Obstetrician and Gynecologists. ACOG practice Bulletin No 110: Noncontraceptive uses of hormonal contraceptives. Obstet Gynecol. 2010; 115(1): 206-218)
1.Menstrual cycle regularity
2.Treatment of menorrhgia
3.Treatment of dysmenorrhoea
4.Inducing amenorrhoea for life style considerations
5.Treatment of premenstrual syndrome
6.Prevention of menstrual migraines
7.Decrease in risk of endometrial cancer, ovarian cancer, colorectal cancer
8.Treatment of acne or Hirsutism
9.Improved bone mineral density
10.Treatment of bleeding due to Leiomyoma
11.Treatment of pelvic pain due to endometriosis
Sunday, January 5, 2014
Re-definition of menstrual disorders
Terminology abandoned by FIGO (adapted from reference Munro et al. Int J Gynaecol Obstet 2011; 113: 3-13)
Out of date terminology
1. Dysfunctional uterine bleeding/ functional uterine bleeding
2. Menorrhgia (including idiopathic menorrhgia, essential menorrhgia, ovulatory menorrhgia, anovulatory menorrhgia, polymenorrhgia, epimenorrhagia)
3. menorrhoea (including epimenorrhoea, hypermenorrhoea, polymenorrhoea)
4. Menometrorrhagia
5. Metrorrhagia
6. Metropathia hemorrhagica
7. Oligomenorrhea
8. Uterine haemorrhage
Friday, January 3, 2014
Mitral stenosis and pregnancy
Mitral stenosis is predominantly due to prior rheumatic fever.
Stenotic vulvular lesions are less well tolerated in pregnancy with maternal mortality rate greater than 10%.
Poor prognostic signs are presence of symptoms pre-pregnancy and severe stenosis (valve area <1 cm2).
Patients usually present with breathlessness, fatigue or acute pulmonary oedema.
Due to dilatation of the left atrium, they often have atrial fibrillation. Tapping apex beat, loud first heart sound and mid diastolic murmur are features of mitral stenosis.
Patients with atrial dilatation may require prophylactic heparin and those with atrial dilatation require therapeutic heparin.
Thursday, January 2, 2014
Fetal thyroid function
TSH (thyroid stimulating hormone) is a glycoprotein.
TSH stimulates the release of thyroxine T4 and tri-iodothyronine T3.
The major action of thyroid hormones is to stimulate oxygen consumption.
The developing thyroid is first recognized as a thickening on the floor of the pharynx at around four weeks gestation. However, it does not begin to function until the end of the first trimester. Fetus uses maternal thyroid hormone T4 which crosses placenta in small amounts only during first trimester.
Fetal pituitary starts to secrete TSH in the second trimester and level increases steadily between 20 abd 30 weeks of gestation.
Fetal thyroid gland starts to secrete T3 and T4 from 10 weeks gestation onward.
From this point onwards, the fetal thyroid axis is independent and little relationship between maternal and fetal levels.
Wednesday, January 1, 2014
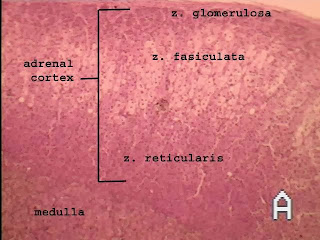
Adrenal cortex
The adrenal cortex can be divided into 3 zones.
Zona glomerulosa secretes aldosterone.
Intermediate layer Zona fasiculata forms the greater part of the cortex and is probably a non-secreting zone of reserve cells.
Zona reticularis secretes cortisol.
Cortisol secretion is under the control of ACTH. The circadian rhythm is maintained by pituitary ACTH secretion and mediated by corticotrophin releasing factor secretion from median eminence of the hypothalmus.